News
Vol.26 (2023/01/25) Global infection trends and domestic antibody possession rate / Positive antibody test rate at our clinic / After-effects of COVID-XNUMX on the nervous system / COVID-XNUMX classification changed to "Category XNUMX"
Life under the coronavirus pandemic will soon enter its fourth year, and we are now in the "eighth wave" of the pandemic, with the possibility of anyone becoming infected at any time.
While the legal classification of this infectious disease is being debated, we are also learning more about the after-effects of infection.
This time, we will be checking infection trends both domestically and internationally, and providing the latest information on the aftereffects of COVID-19 on the nervous system.
[1] Global situation report on COVID-19
A decrease in the number of infected people and deaths has been observed worldwide.
Figure 1: Trends in COVID-2023 infections and deaths worldwide by week or WHO region as of January 1, 8
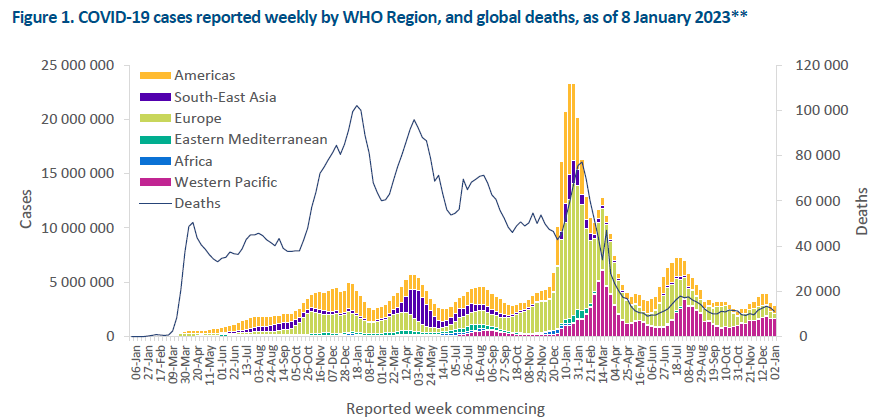
Source: COVID-19 Weekly Epidemiological Update (WHO) January 2023, 1
https://www.forth.go.jp/topics/20230112_00001.html
[9] Large regional differences in coronavirus antibody possession rates in Japan (46% to XNUMX%)
The Ministry of Health, Labor and Welfare announced on the 4th that the antibody possession rate (preliminary figure) of people nationwide who are infected with the new coronavirus was 26.5%. There were large regional differences by prefecture, ranging from 9% to 46%, suggesting that this may be affecting the current infection situation. There was also a tendency for the possession rate to decrease with age.
The survey was carried out from November 11 to 6. With the cooperation of the Japanese Red Cross Society, blood from 13 men and women aged 16 to 69 who donated blood from across the country was examined for the presence of antibodies obtained from viral infection.
保有率の最も高かった地域は沖縄(46.6%)で、大阪(40.7%)、鹿児島(35.2%)、京都(34.9%)、熊本(32.9%)の順だった。最も低かったのは長野(9.0%)で、徳島(13.1%)、愛媛(14.4%)、新潟(15.0%)、岐阜(15.5%)と続いた。
By age, the highest percentage was 16-19 years old (38.0%), and it was over 20% for those in their 30s and 3s. However, the ownership rate decreased as age increased, with the lowest being those in their 60s (16.5%).
Nagano, where the antibody possession rate is below 10%, recorded a record number of new infections in November. Meanwhile, Okinawa, where nearly half of the population has an antibody possession rate, recorded a record number of new infections this summer, but is currently showing a lower trend than the national average.
The previous survey, conducted in February and March in five prefectures - Tokyo, Osaka, Miyagi, Aichi, and Fukuoka - found that antibody possession rates were low, ranging from 2 to 3%.
Source: Regional differences in coronavirus antibody possession rates: 9-46%, possibly influenced by infection situation - Nationwide, 26.5%, Ministry of Health, Labor and Welfare, December 2022, 12 (Jiji Press)
https://www.jiji.com/jc/article?k=2022120400168
[19] Regarding the results of our COVID-XNUMX antibody test
At our hospital, we measure infectious and neutralizing antibodies and compile the results every month.
(We believe this is the only data available from fixed-point observations in Tokyo.)
Since the cutoff value for infectious antibodies is 1, a value of 1 or above is reported as positive. For trends in the number of positive cases with a value of 1 or above, please refer to Figure 2.
Figure 2: Positive rate of antibody tests at Tokyo Midtown Clinic
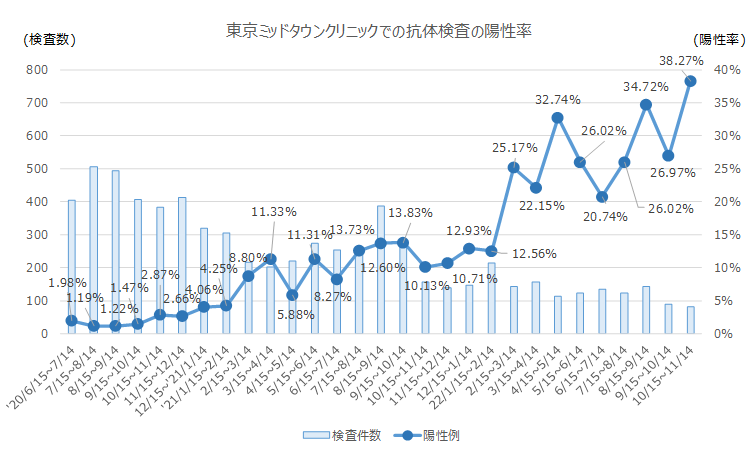
In fact, in cases where the infection was mild, the infection antibody level drops to 0.1 or less after more than a year, and there are cases where the patient is determined to be negative. In cases with no history of infection, the infection antibody level is 0.2 or less, so the data for the number of cases with infection antibody levels of XNUMX or more was recounted.
The results are as shown below (Figure 3), and it is estimated that from August 2022 onwards, more than 8% of people will have had at least one infection in the past.
Figure 3: Changes in the number of COI tests and the percentage of patients with COI values of 0.2 or higher at Tokyo Midtown Clinic

[4] Regarding aftereffects of COVID-19 on the nervous system
This is the latest information on symptoms of the nervous system that are an aftereffect of the new coronavirus.
19) Medical Treatment Guide for COVID-XNUMX
[Post-mortem symptoms of the mental and neurological system]
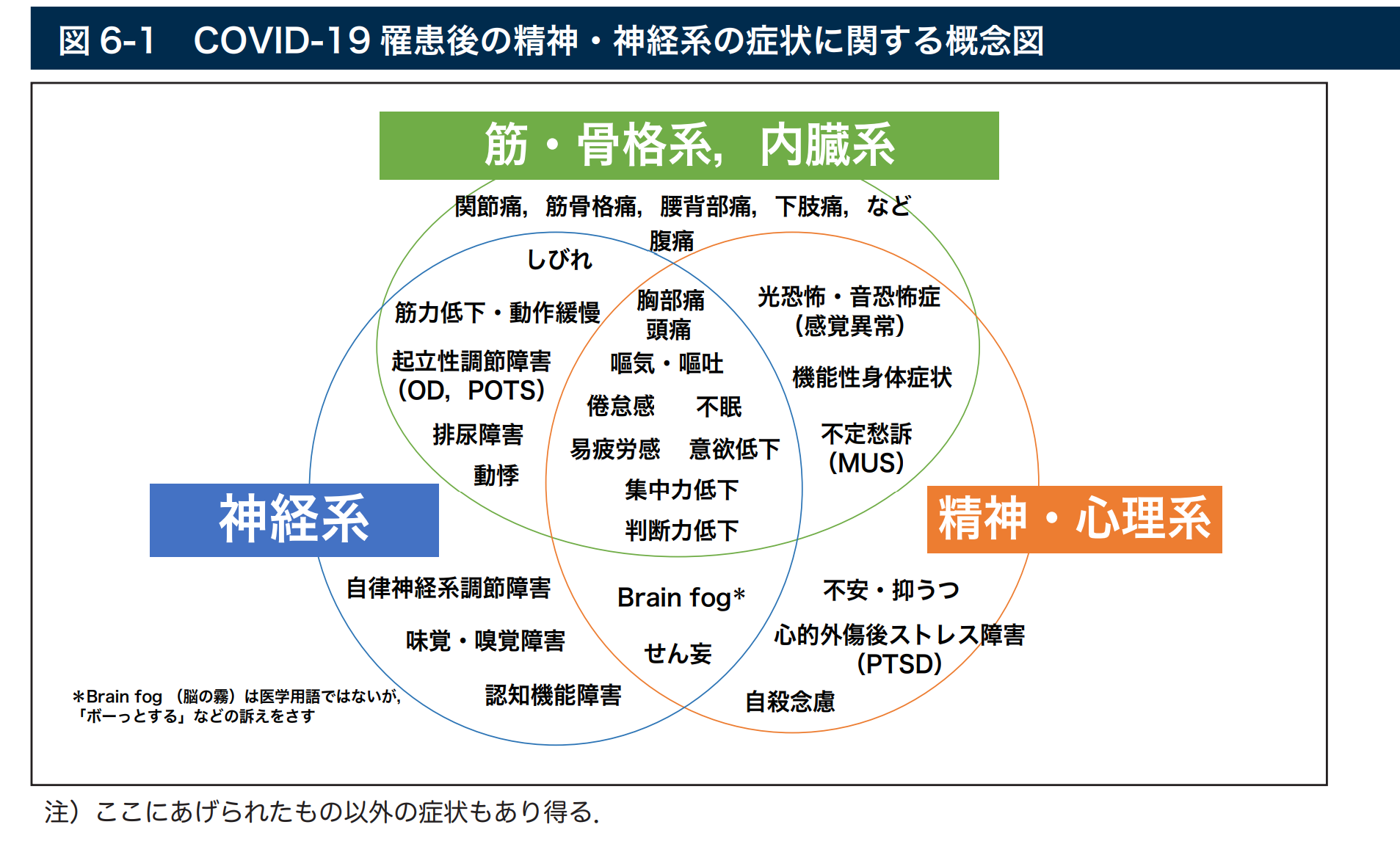
Postmortem symptoms of the mental and nervous system are thought to be partly caused by abnormalities in any of the functional areas (organs) of the central and peripheral nervous system, musculoskeletal system, visceral system, and mental and psychological activity, and in many cases, as shown in the conceptual diagram in Figure 1-XNUMX, symptoms are related to multiple functional areas (organs). In addition, organic damage to various organs and abnormalities in immune responses due to significant inflammatory reactions are also thought to be background factors, and most symptoms are expected to recover over time, and early improvement or prevention of aggravation can be expected with appropriate postmortem follow-up and self-care.
It should be kept in mind that some post-mortem symptoms of the psychiatric and neurological system are based on underlying mental and neurological diseases or predispositions, and that they must be differentiated from exacerbations of the underlying diseases. In addition, it should be kept in mind that in rare cases, post-mortem symptoms may appear that must be differentiated from symptoms of the respiratory and circulatory systems, such as fever and shortness of breath. Pathological conditions in the field of neurology are diverse. Therefore, as a basic guideline for the approach, it is preferable to observe the patient's condition for a certain period of time after the illness with the doctor in charge or the family doctor, rather than immediately referring the patient to a specialist or general hospital. In addition, even if psychological factors are strongly suspected, there is a possibility that anxiety will increase due to a sudden referral to a psychiatrist, so it is not necessary to immediately recommend a psychiatric consultation unless it is urgent.
[Frequency and cause (mechanism)]
Among the post-mortem symptoms related to the psychiatric and neurological systems, fatigue and easy fatigability are commonly reported. According to the UK Office for National Statistics, the prevalence of COVID-19 is 11.9% at 40 weeks after infection, but the incidence varies depending on the literature, ranging from approximately 80% to 90%, and in some cases exceeding 19%. In addition, it has been reported that the incidence of symptoms does not depend on the severity of COVID-XNUMX.The underlying factors suggested to be involved include the central nervous system, peripheral nervous system, and psychological factors, and the main mechanisms reported to involve the central nervous system include 1) damage to glial cells due to a long-term immune response, and 2) impaired function of the blood-brain barrier and increased vascular permeability.
In addition, symptoms such as "brain fog" and impaired executive function and concentration are said to be characteristic symptoms centered on the central nervous system. It has also been suggested that the significant inflammatory response may induce hypercoagulability, which may lead to increased risk of cerebral infarction and cerebral hemorrhage due to the increased likelihood of blood clots forming, and caution is required. The main post-mortem symptoms of the mental and psychological system include anxiety, restlessness, depression, and PTSD (post-traumatic stress disorder). The prevalence at one month after hospitalization was reported to be 1%, and the prevalence at three months in a retrospective study of a large-scale cohort in the United States was reported to be 56% (of which 3% were new cases), and these may also be background factors for the fatigue and fatigue mentioned above.In addition to these, various pains and numbness caused by organic disorders of the skeletal muscles and peripheral nerves, and orthostatic dysregulation (OD, postural orthostatic tachycardia syndrome, etc.), as well as disuse muscle weakness associated with long-term hospitalization (bed rest), and fatigue and easy fatigability caused by post intensive care syndrome (PICS), etc. must also be taken into consideration.
Source: COVID-19 Medical Treatment Guide (Ministry of Health, Labor and Welfare)
https://www.mhlw.go.jp/content/000860932.pdf
2) Survey on the actual "after-effects of COVID-19" among Japanese people: Which gender is more affected in daily life?
[Common symptoms include fatigue, depression, brain fog, and headaches]
The subjects of the analysis were long COVID patients who visited an outpatient care facility (Hirahata Clinic) in Tokyo between January 2020, 1 and October 6, 2021, and had symptoms that persisted or developed more than 10 days after the onset of COVID-2. Of these, 19 patients had symptoms that persisted or developed more than 28 days after the onset of COVID-1,898, and 7 patients were excluded after excluding 1,891 patients for whom the data necessary for analysis was missing. The mean age was 37.8 ± 12.2 years, and 59.7% were women. The timing of visits was 1% in the first wave of the pandemic, 1.8% in the second wave, 2% in the third wave, 5.9% in the fourth wave, and 3% in the fifth wave. 41.8% had completed vaccination.The impact of Long COVID symptoms on activities of daily living was evaluated using a performance status (PS) score out of 10, with the average being 3.1 ± 2.4 points. PS is scored as 0 if there is no impact on daily life at all, and 10 if the patient is bedridden and completely dependent all day. A score of 3, close to the average, corresponds to a condition in which the patient needs to take several days off work per month due to symptoms. In fact, only 23.7% of the subjects were still working as before the disease, 14.2% were working with reduced hours, and 20.9% were on leave or had retired or been fired (8.3% were not working, and 32.8% were unknown).
訴える症状の数は平均8.4±3.2種類であり、頻度の高い症状は、倦怠感(90.3%)、抑うつ(81.2%)、ブレインフォグ〔頭がぼんやりして記憶力などが低下した状態(76.2%)〕、頭痛(71.2%)、呼吸困難(68.9%)、不眠症(63.8%)、動悸(61.7%)、体の痛み(60.6%)、嗅覚障害(52.4%)、食欲不振(50.6%)、味覚障害(45.2%)、脱毛(44.8%)などだった。
PSスコアが6点(週の50%以上を休息している場合)以上をPSが特に低下した状態と定義すると、24.0%が該当。年齢や性別、受診時期(パンデミック第何波に当たるか)、ワクチン接種状況、就労状況などを調整後に、PS6点以上であることと関連する因子を検討すると、女性〔β=0.27(95%信頼区間0.08~0.47)〕、時短勤務者〔通常勤務者を基準にβ=1.59(95%信頼区間1.27~1.91)〕、休職中または退職・解雇後〔同3.64(3.35~3.93)〕、非就労〔同1.67(1.22~2.21)〕が有意な関連因子として抽出された。
The authors concluded that "our findings suggest that women are more likely to have a decreased PS during long COVID disease, and we also found a significant association between employment status and PS," and stated that "further research is needed to understand the overall characteristics of long COVID patients in Japan." (HealthDay News, January 2023, 1)
Source: Survey on the actual situation of "COVID-2023.1.14 aftereffects" among Japanese people: Which gender is more affected in daily life? (Diamond Online/Health Day News) January XNUMX, XNUMX
https://diamond.jp/articles/-/316050
3) How brain fog works
Long-lasting neurological and behavioral problems have been reported even after recovery from COVID-40. One of these symptoms is "brain fog," which can cause disorientation (not knowing people, time, or place), memory loss, chronic headaches, and numbness, and affects nearly XNUMX% of COVID-XNUMX patients.
Human nerve cells (neurons) consist of a cell body, a long axon, and spider-like dendrites. Synapses, or connections between nerve cells, allow nerve cells to communicate with each other.
Scientists at the Karolinska Institute in Sweden infected brain organoids (small laboratory-grown brain tissues) with the new coronavirus and found that it promoted the destruction of synapses, the connections between nerve cells (neurons). The findings were published in the academic journal Molecular Psychiatry on October 2022, 10. They concluded that excessive pruning of synapses, which connect neurons, may be causing brain fog in patients with COVID-5 sequelae. "Perhaps this is one of the reasons why various neurological symptoms are seen even long after recovery from COVID-XNUMX," says Dr. Schneider. "It was really shocking to see how a tiny amount of virus spread so quickly in the brain organoids and how so many synapses were eliminated."
■ Synaptic pruning is essential for learning
The brain is made up of a dense, dynamic network of nerve cells that communicate through their endings, called synapses, which change as we learn. "Synapses are basically how nerve cells talk to each other and transmit information from one part of the brain to another," says Dr. Schneider. "Synapses are involved in all brain functions, including memory, motor control and emotions, and the way they are connected is constantly changing. "That's how we learn."Neurons with frequent communication have many synapses, while neurons with little or no communication have fewer synapses. This is because synapses are pruned by immune cells called "microglia." In some parts of the human brain, microglia make up 17% of the cell population. Microglia travel around the brain and clean up the brain by eating dead cells and removing unnecessary synapses.
Synaptic pruning is most active in the developing brain, such as in fetuses and infants, but continues throughout life in healthy brains and is necessary for the formation of new memories and the erasure of memories that are no longer needed. It is also essential when the brain is recovering from injury, strengthening synapses to relearn lost skills and removing synapses that no longer function.
■ Research into neuronal damage using brain organoids
Using brain organoids, the researchers found that the new coronavirus does not directly prune synaptic connections, but activates microglia.
"We found that after infection with COVID-19, microglia somehow mount an immune response and eat more synapses than usual," he says.Excessive pruning of synapses can be harmful and has been linked to neurodevelopmental disorders such as schizophrenia and neurodegenerative diseases such as Alzheimer's and Parkinson's.
If excessive synapse elimination, as occurs in brain organoids after COVID-19, were to occur in the human brain, it could disrupt essential connections and potentially explain why people with COVID-19 suffer long-term neurological symptoms.
"Excessive removal of synapses would be expected to affect the ability to form new memories and recall existing ones, and may explain the decline in brain function seen in brain fog," he says.This is consistent with the results of a study by the National Institutes of Health (NIH) published in the journal Brain on July 2022, 7. The study found that even if the new coronavirus does not directly invade the brain, antibodies produced in response to the virus can attack cells on the surface of blood vessels in the brain, causing damage and inflammation and activating microglia.
■ Does loss of synapses cause brain shrinkage?
A British study published in the academic journal Nature on March 2022, 3, showed that even mild COVID-7 infection can damage the brain through a loss of gray matter, causing changes equivalent to 10 years of aging. Gray matter is located in the outer layer (cortex) of the cerebrum and cerebellum and is essential for controlling movement, memory, and emotions.
"We still don't know what causes the reduction in grey matter volume and thickness that we see on MRI," says neuroscientist Gwenaël Douault of the University of Oxford in the UK, who led the study.
He noted that the loss of synapses shown in this study is likely only a small part of what causes the grey matter changes, and further studies combining imaging and tissue sections are needed to uncover other factors that lead to brain shrinkage.
Source: Coronavirus post-traumatic brain fog: Synaptic destruction may be a contributing factor (National Geographic, December 2022, 12)
https://www.nikkei.com/article/DGXZQOUD079ND0X01C22A2000000/
[5] Moves to change to "Class XNUMX" under the Infectious Diseases Control Act
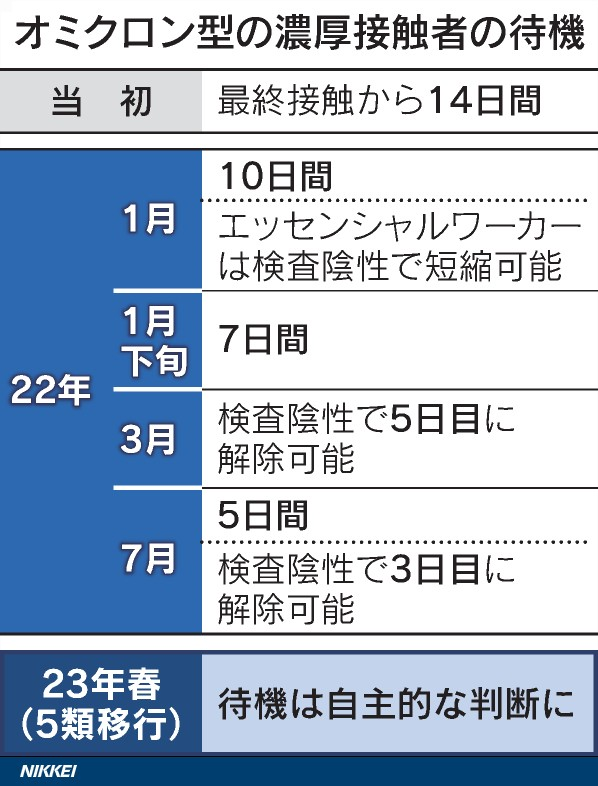
Starting this spring, the government will change the classification of the new coronavirus under the Infectious Diseases Control Act to "Class 5," the same as seasonal influenza. There will no longer be legal restrictions on people's behavior. There will be no uniform request for infected people or those in close contact with them to stay at home, and people will be required to make their own decisions about the virus, just like with the common cold.
Figure 4: Changes in waiting period for close contacts
The Infectious Diseases Act classifies infectious diseases into categories such as Class 1 to 5 and "designated infectious diseases" based on factors such as pathogenicity. COVID-2 is a "new influenza-like infectious disease," while Class XNUMX and above, which includes tuberculosis, are subject to stricter measures.
For example, Article 44-3 of the law stipulates that prefectures may ask infected or suspected infected people to refrain from going out. They may also recommend hospitalization and restrict employment.
At the start of the outbreak, public health centers narrowed down close contacts suspected of infection based on behavioral history and other factors in epidemiological surveys under Article 15. Now that the number of infected people has increased, the decision is left to the discretion of businesses and individuals, with the exception of contacts within households.
The specific treatment is indicated by the Ministry of Health, Labor and Welfare in administrative notices to local governments. The definition of close contact has been changed according to the characteristics of the virus. Currently, it applies to those who have spent "2 minutes or more at a distance of about 1 meter" without a mask with a positive person within two days before the onset of symptoms, which is considered to be a high risk of infection.
In principle, infected people will be required to stay at home or in a lodging facility to avoid going out for seven days, while close contacts will be required to stay at home for five days. These regulations will be abolished if the situation is moved to Class 7. Local governments will also no longer have the authority to recommend hospitalization or restrict employment.
Administrative tasks such as arranging hospitalization and monitoring the health of patients during waiting periods will be gradually reduced while being maintained as necessary. Monitoring the health status of patients will become part of the normal duties of medical institutions.
Medical treatment, which was previously limited to certain areas such as fever clinics, will be gradually transferred to all medical institutions. As a common, everyday illness, special crisis responses will be scaled down. Rules such as wearing masks, which the government has required separately from laws and regulations, will also be significantly relaxed.
Recent data shows that the mortality rate has already fallen to the same level as seasonal influenza. There has been growing criticism that the strict measures are preventing socio-economic activities from returning to normal.
It is not acceptable to let our guard down. We are currently in the eighth wave of the epidemic, with some days seeing a record high of over 8 deaths a day, mainly among the elderly. To ensure a smooth transition, we need to maintain the infrastructure that allows patients to receive the medical care they need.
Source: Coronavirus "Class 5", waiting period lifted for close contacts, measures to be decided independently (Nikkei Newspaper, January 2023, 1)
https://www.nikkei.com/article/DGXZQOUA20BNL0Q3A120C2000000/
*The content of this page is current as of July 2023, 1.