News
Vol.13 (September 2020, 9) Results of antibody tests at our clinic, trends of infected people in Japan and the world, learning from past pandemics, the latest drugs, treatments, and vaccines, etc.
The number of new COVID-100 infections in Tokyo is still at over XNUMX, but looking at the data, it appears that we have passed the second peak.
However, that does not mean we can relax our infection prevention measures. Learning from the Spanish flu, which was prevalent over 100 years ago, I believe we need to prepare for this fall and winter.
In this issue, we will take an overview of the current situation regarding the new coronavirus infection, while reaffirming the current status of development of treatments, cures, and vaccines. We will also provide information on coronavirus testing by family doctors, which is being promoted by the Ministry of Health, Labor and Welfare, and the latest testing information.
- Topics
1. About the results of the COVID-XNUMX antibody test at our clinic
2. Statistics from Japan suggest that the second wave has passed.
4. This is a report from a consulting firm that looked into the economic impact.
5. What we can learn from past pandemic information (Spanish Flu)
6. Current status of treatments and cures, from an article in the New York Times
[1] Results of COVID-19 antibody tests at our clinic
当クリニックでは発熱や咳などの症状がない(過去2週間以内にもなかった)方を対象に実施しておりますが、7月15日から8月14日の間の陽性率は、506例中6例(1.18%)でした。また、6月15日の検査開始からの通算では、911例中14例(1.54%)でした。
Many people have no clear symptoms, so it seems that there are quite a few asymptomatic infections.
[2] Statistics from Japan suggest that the second wave has passed
According to a report from the Ministry of Health, Labor and Welfare, as of September 70,051th, the number of infected people (positive cases) announced by each local government was tallied, bringing the total number of infected people since the initial announcement to 1,348, with XNUMX deaths.
The second wave, which began around the end of June, saw a large number of patients, but the number of deaths has clearly decreased.
(Figure 1) Number of new infections by day (as of September 9)
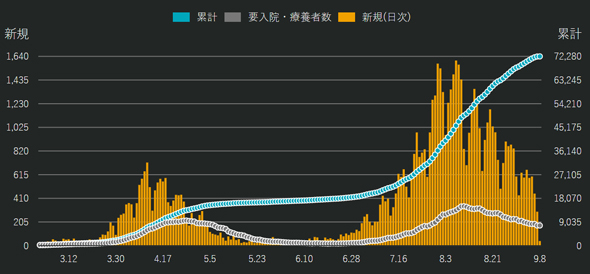
Source: News Digest: COVID-19: Latest infection status map for Japan
https://newsdigest.jp/pages/coronavirus/
(Figure 2) Number of new deaths by day (as of September 9)
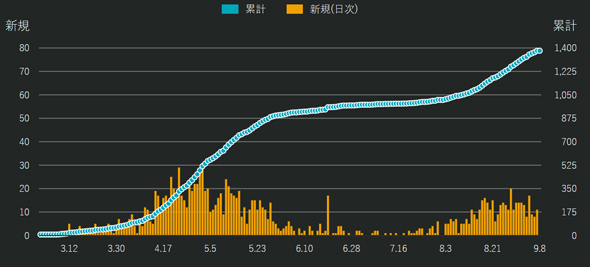
Source: News Digest: COVID-19: Latest infection status map for Japan
https://newsdigest.jp/pages/coronavirus/
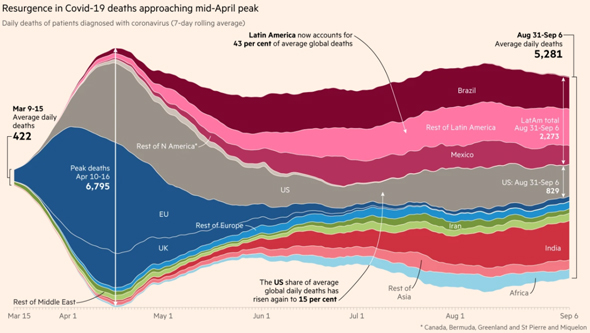
[3] Global situation: America and South America are at the forefront
The number of new deaths is high in Brazil, Latin America, the United States, and India, and is clearly decreasing in the EU and the UK. The overall number of deaths is not yet showing any signs of decreasing.
(Figure 3) Trends in the number of daily deaths worldwide
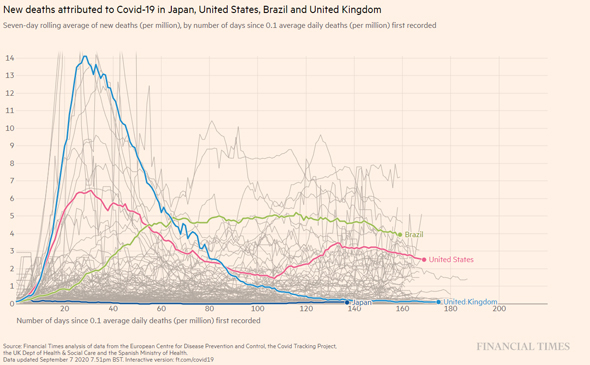
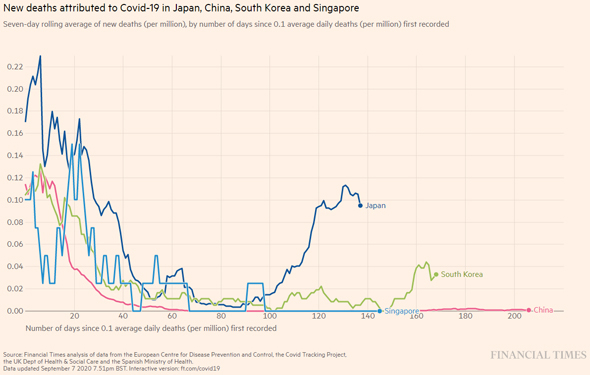
This is a graph of the number of new deaths by country. Japan's numbers are much lower, and it is clear that the number of deaths in the UK has dropped dramatically.
However, if we focus on East Asia, Japan has a relatively low number of deaths compared to China, Singapore, and South Korea.
(Figure 4) Number of new deaths by country (Comparison between the United States, Brazil, the United Kingdom, and Japan)
(Figure 5) Number of new deaths by country (Comparison of Japan, China, South Korea, and Singapore)
The number of excess deaths compared to normal years is high in Europe, the United States, and South America, but has not increased in Asia, including Japan.
(Figure 6) Excess deaths by country

Source of all graphs in this section: Financial Times "Coronavirus tracked: the latest figures as countries fight Covid-19 resurgence"
https://www.ft.com/content/a2901ce8-5eb7-4633-b89c-cbdf5b386938
[4] This is a report from a consulting firm that looked into the impact on the economy.
We present the results of a survey compiled by consulting firm McKinsey & Company on the impact of COVID-19 on the economy and consumer sentiment.
The data is only up to July, but in China, India, the United States and other countries, many people are optimistic about the future of the economy (top of the graph), while Japan has the strongest pessimistic tendencies (bottom of the graph).
However, if we look at the days, the pessimistic tendency has decreased slightly since July.
As the second wave subsides, this trend may change again.
(Figure 7) Changes in consumer sentiment by country
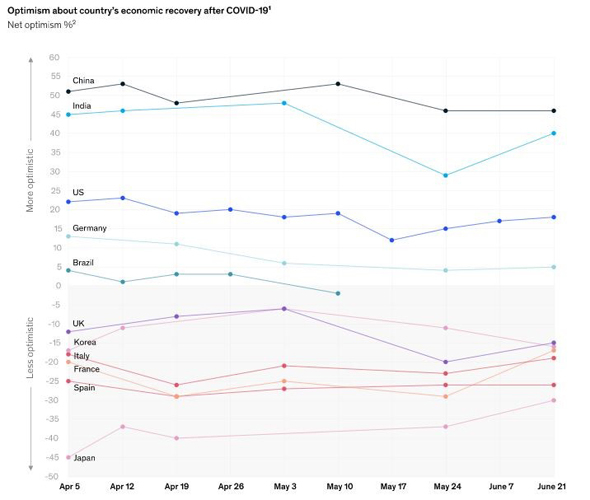
Source: McKinsey&Company: Consumer sentiment and behavior continue to reflect the uncertainty of the COVID-19 crisis
https://www.mckinsey.com/business-functions/marketing-and-sales/our-insights/a-global-view-of-how-consumer-behavior-is-changing-amid-covid-19
[5] What we can learn from past pandemic information (Spanish flu)
Looking back at the course of the Spanish influenza (also known as the Spanish flu), which caused a global pandemic in the early 20th century, we can see how important it is to take measures this fall and winter.
- What is the Spanish Flu?
The Spanish Influenza was the largest scientifically verifiable influenza pandemic in history, spreading worldwide from around March 1918 to around 3.
There are various accounts of the statistics, but during this time, more than one-third of the world's population at the time, who was between 18 and 20 billion people, were infected, tens of millions (said to be roughly 1 to 3 million) died, and the mortality rate (the ratio of the number of deaths to the number of people who became infected) is estimated to be over 2%.
Because this epidemic occurred during World War I, it caused severe damage to soldiers of the participating countries and had a major impact on the course of the war.
Each country tried to keep the influenza epidemic secret so their enemies would not realize that it was weakening their military strength, but in Spain, which was not involved in the war, there was no information control, and the epidemic in the country was widely reported around the world.
Because reports had emerged that the King of Spain and his ministers had also contracted influenza, the pandemic was perceived as having originated in Spain, and was therefore named after the country.
- Where did the Spanish flu originate?
The first clearly recorded epidemic that led to the Spanish flu occurred in the United States in March 1918, and this is generally considered to be where the epidemic began.
However, the presence of a record does not necessarily equate to the true location of origin.
In particular, China is the country where Asian and Hong Kong influenza outbreaks occurred, and where human infections with avian influenza A(H5N1) and A(H7N9) viruses were first reported, leading to the view that the Spanish flu may have also originated in China.
There are also theories that it originated in Europe (France, etc.) or Africa.
- The causative agent of Spanish influenza
The causative virus of the Spanish flu is known to be an influenza virus of the subtype A(H1N1).
This virus is thought to have been created by a reassortment of human and avian viral genes, and in 1918 it could be called a "new type of influenza."
- The Spanish Flu in the United States
The epidemic that occurred in the spring of 1918 is called the first wave of Spanish influenza (spring wave).
In the first wave, although the number of infected people was high, the mortality rate was not very high.
This first wave temporarily slowed down around the summer of the same year.The epidemic that began around September 1918 is called the second wave, and the epidemic from early 9 onwards is called the third wave.
It is known that especially during the second wave, there were many patients who developed pneumonia and became seriously ill, and many who died.Industrial functions declined due to the large number of factory workers absenteeizing, and many hospital doctors and nurses, telecommunications company employees, police officers, railway workers, garbage collectors, and undertakers fell ill with influenza, causing a significant decline in public services.
In some households, there was no adult left who was physically able to work or do housework, and with income and food cut off, the whole family was unable to leave the house, so volunteers went around cooking soup kitchens and delivering meals.It is not clear why the mortality rate was higher in the second wave compared to the first wave.
Various possibilities have been pointed out, including the virus mutating to become highly pathogenic for humans, or the second wave coinciding with the cold season when influenza normally spreads.There are many statistics on the damage caused to the United States during the Spanish Influenza epidemic, including that more than a quarter of the total population, or more than 1918 million people, contracted the flu between 1919 and 1, and 4 people died (including 2,500 "excess deaths," or the number of people who died above normal due to the pandemic).
The Spanish flu gradually died down in the United States, and as most of the population developed immunity to it, its pathogenicity decreased and it transitioned into seasonal influenza.
- The Spanish Flu in Japan
In Japan, the Spanish flu epidemic began in late August 1918 (Taisho 7) and became a nationwide pandemic by November.
The first storm-like outbreak began to slow down around December.
At the time, the Ministry of Home Affairs' Health Bureau reported that the total number of patients during the first epidemic was 5,719, out of a total population of 1 in Japan.
This means that approximately 37% of the population had the flu during this period.
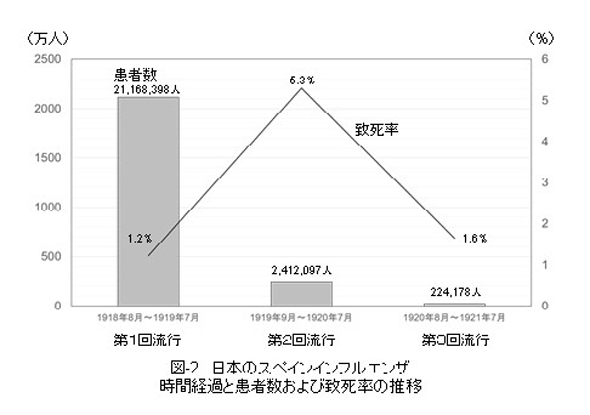
Of these, the total number of deaths is estimated to be 25, so a simple calculation gives a mortality rate of 7%.その後、第2回流行(1919年9月~1920年7月)では総患者数241万2千人、総死亡者数12万8千人(致死率5.3%)、第3回流行(1920年8月~1921年7月)では総患者数22万4千人、総死亡者数3,698人(致死率1.6%)と記録されています。
Judging from the total number of patients, it may be better to consider the third outbreak as having already transitioned into seasonal influenza.(Figure 8) Changes in the number of patients and fatality rate of Spanish influenza in Japan over time
- ◆The Yahagi Warship Incident
The Yahagi was a light cruiser based in Kure, and while carrying a total of 469 people, it stopped in Singapore in November 1918, where a crew member who disembarked briefly brought the influenza virus with him.
Influenza spread explosively inside the confined space of the ship, causing nurses and military doctors to fall ill. Ultimately, 306 people (65%) fell ill, of whom 48 died (a fatality rate of 16%).
However, some of the passengers who boarded from Singapore had previously contracted Spanish flu and recovered, and did not become ill on board the ship.
This incident also teaches us that once you have had the disease, you become immune to it and will not get it again.
- ◆Infectious disease prevention measures at the time
In 1918, viruses had not yet been discovered, but it was thought that pathogens that invade the respiratory tract and are released during coughing and sneezing were the source of infection.
It has been recorded that various infection control measures were taken.
For example, some U.S. government authorities have recommended that citizens refrain from coughing or sneezing in public and wear masks.
He also has a record of ordering the closure of schools, churches, theaters and other places of mass entertainment.
The city of St. Louis, which proactively implemented public health measures such as closing schools, was successful in preventing the spread of infection, but there are records of the infection spreading in Philadelphia, where no such measures were taken, and this example is still often cited when considering the importance of public health intervention.In Japan, the Ministry of Home Affairs' Health Bureau published "Tips for Preventing Epidemic Colds" in January 1919.
It says that "when you cough or sneeze, tiny, invisible bubbles are blown into the air, and if you inhale them you will contract the disease," so it is important to "stay away from sick people or those who are coughing," "avoid entering places where there are a lot of people (theaters, moving pictures, trains, etc.)," and "cover your nose and mouth with a handkerchief or towel when coughing or sneezing."
In addition, if you catch the flu, it is recommended that you "rest immediately" and that "if possible, stay in a separate room from the sick person and wear a mask when entering the hospital room" (some parts translated into modern language).
This is almost identical to what is currently recommended as "cough etiquette," and it is surprising that the same modern-day influenza prevention measures were recommended 100 years ago.What concerns me is that the infection control measures at the time barely mentioned hand hygiene (hand washing).
At the time, there was not enough running water, soap, or alcohol-based disinfectants available.
Source: Cabinet Office, Past Pandemic Review: December 2018 and 12, 17,25, article by Professor Akihiko Kawana of the National Defense Medical College
https://www.cas.go.jp/jp/influenza/kako_01.html
As the paper states, the influenza prevention measures recommended 100 years ago are similar to current COVID-XNUMX prevention measures. We should continue to take basic actions such as washing our hands, coughing etiquette, and avoiding the "three Cs" to prepare for the next wave.
[6] Current status of treatments and cures, from a New York Times article
Although Japan is over the second wave, the virus is still in its epidemic phase worldwide, and if past examples are any indication, we need to prepare for this fall and winter. How far has research into treatments and cures progressed?
See the article compiled by the New York Times.
(Figure 9) Drugs and treatments for COVID-21 (summary of XNUMX types)
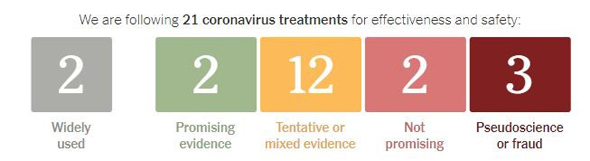
Source: The NewYork Times: Coronavirus Drug and Treatment Tracker
https://www.nytimes.com/interactive/2020/science/coronavirus-drugs-treatments.html
- Widely used: Artificial respiration, etc. are featured.
- Promising evidence: Remdesivir and corticosteroids. Both are treatments for severe cases.
- Possible options with tentative or mixed evidence: Avigan (Favipiravir), MK-4482, synthetic ACE2, Ivermectin, Oleandrin, convalescent serum from infected patients, monoclonal antibodies (Eli Lilly, USA), interferon, cytokine inhibitors, hemodialysis (cytokine removal), and anticoagulant therapy.
- Not promising: HIV drugs (Lopinavir and Ritonavir), Chloroquine
- Do not do this: Drink bleach or disinfectants, expose yourself to UV rays, or actively use lotions or soaps that contain silver.
- ◆There have also been reports that statins, a typical treatment for hypercholesterolemia, may be effective.
In summary, statins:
- It has the effect of preventing the new coronavirus from entering cells by changing the ACE2 receptor, CD147 receptor, and lipid raft structure (one of the entry points for bacteria and viruses).
- Activates autophagy (the process of breaking down one's own proteins) to regulate the proliferation and degradation of viruses
- anti-inflammatory
- Inhibits activation of coagulation reaction
Apparently there is.
Source: Statins: Could an old friend help the fight against COVID-19?J Pharmacol.2020;10.1111/bph.15166.
doi:10.1111/bph.15166
https://bpspubs.onlinelibrary.wiley.com/doi/full/10.1111/bph.15166Such verification is being conducted around the world, and further research results are eagerly awaited.
[7] Latest trends in vaccine information
Following the treatments and cures, we will also introduce vaccines.
(Figure 10) COVID-XNUMX vaccine
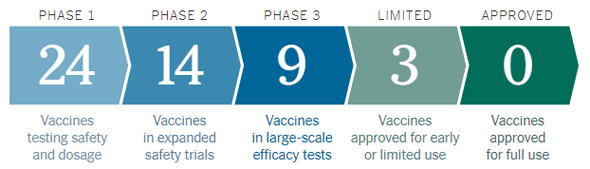
Source: The NewYork Times: Coronavirus Drug and Treatment Tracker
https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html
Limited use (LIMITED)
- China CanSino Biologics: Use in the Chinese military and Phase 3 trials in Saudi Arabia and Pakistan.
- Russia's Gamaleya Research Institute: The president has already given permission for its use under the name Sputnik V, but it will apparently only be implemented from the third phase.
- China Sinovac: Has undergone phase 3 trials in Brazil and Indonesia and has been approved for limited emergency use.
Phase 3 trial (PHASEXNUMX)
Moderna (messenger RNA vaccine), Pfizer etc. (messenger RNA vaccine), AstraZeneca, China Sinopharm, and BCG vaccine.
The situation may change again next month.
[8] The BCG vaccine appears to be effective after all
As shown in Figure 10, a randomization study was conducted using the BCG vaccine in elderly subjects.
The BCG group had a clear reduction in new respiratory infections and viral respiratory infections, without any side effects.
However, the Japanese BCG strain is superior, and there is currently not enough evidence to make a definitive statement as to whether re-administration is necessary for elderly people in Japan.
(Figure 11) Summary of the effectiveness of BCG vaccine in preventing infectious diseases in the elderly
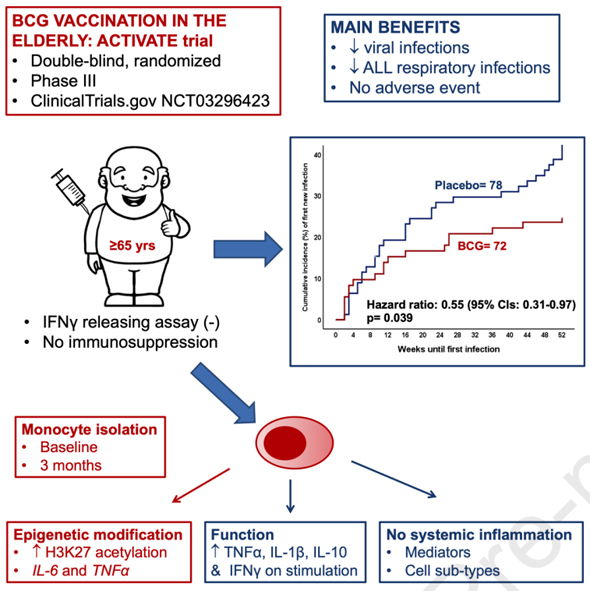
Source: Cell:ACTIVATE: RANDOMIZED CLINICAL TRIAL OF BCG VACCINATION AGAINST INFECTION IN THE ELDERLY August 31, 2020DOI:https://doi.org/10.1016/j.cell.2020.08.051
https://www.cell.com/cell/fulltext/S0092-8674(20)31139-9
[9] The presence of antibodies may or may not prevent reinfection.
During the Spanish flu warship Yahagi incident, people who boarded the ship from Singapore and had been infected once did not become infected a second time, and this has also happened with the current coronavirus infection.
Of the 122 people who went out on the fishing fleet, 85% were infected with COVID-19, but those who had previously been infected and had antibodies did not become infected. Neutralizing antibodies were confirmed, which was thought to be effective in preventing reinfection.
Separately, it was reported that Hong Kong was the first place in the world to confirm a case of reinfection with coronavirus.
CNN News (August 2020, 8) https://www.cnn.co.jp/world/25.html
A 33-year-old man living in Hong Kong tested positive for the new coronavirus on March XNUMX and experienced symptoms of cough, sore throat, fever and headache for three days, but later recovered.
However, when he returned from Spain via the UK on August 8, he tested positive again in the PCR test taken at the airport.
The man was taken to hospital but did not show any symptoms.
Genetic analysis of the viruses from the two infections revealed that the first was close to strains originating from the United States and the United Kingdom, while the second was close to different strains originating from Switzerland and the United Kingdom.
Some people may get the flu twice a year, and if the coronavirus mutates into a different strain, it could be possible for a person to become reinfected depending on their immune response.
It may be necessary to administer multiple coronavirus vaccines and to change the vaccine strain depending on the time of year.
[10] Family doctors will begin offering coronavirus testing
Although research into treatments and cures, as well as the development of a vaccine, is progressing, it will still take some time before these are widely available. Meanwhile, the Ministry of Health, Labour and Welfare has begun to strengthen the medical system for those suspected of infection. In preparation for this fall and winter, please check the situation in your area for yourself.
On the 4th, the Ministry of Health, Labor and Welfare announced a new medical system in which from October onwards, people suspected of being infected with the new coronavirus will seek medical advice from local medical institutions such as their family doctor.
As part of efforts to strengthen outpatient and testing systems in preparation for a simultaneous influenza epidemic, the government will make it possible for patients with fevers to be tested promptly at local medical institutions. On the same day, the government notified prefectures and other local governments in a document calling for the establishment of such systems.Until now, the main point of contact for consultations has been the consultation centers for returnees and contacts set up at public health centers and other locations, but their functions have basically been reduced and they will mainly be responsible for providing information to medical institutions as "examination and consultation centers" (provisional name).
The aim is also to reduce the burden on public health centers, reflecting the lessons learned from the first wave, when public health centers became overwhelmed and some patients were unable to get tested.Under the new system, local governments will designate clinics and other facilities that can perform tests as "medical institutions for treatment and testing (provisional name)." People who suspect they may be infected will basically consult with a nearby medical institution by phone. If the institution is able to perform tests, they can make an appointment and get tested.
If the institution you are consulting does not offer tests, ask them to direct you to a medical institution that offers tests. Local medical institutions should be aware of the locations and opening hours of medical institutions that offer tests. In some areas, the names of medical institutions that offer tests can be found on the local government website. Tests can still be taken at local outpatient and testing centers set up by local medical associations, etc.
Source: From next month, those suspected of having coronavirus will be asked to consult their "family doctor"... Reducing the burden on public health centers: 2020/09/04 Yomiuri News
https://www.yomiuri.co.jp/medical/20200904-OYT1T50312/
[11] Testing methods at clinics
PCR tests are the standard test, but it generally takes more than a day for the results to become available, and the inability to decide what to do during that time may be causing medical and economic stagnation.
It will be important that future coronavirus tests will provide results within 2-3 hours so that decisions can be made immediately.
Tests that can confirm the presence of the virus include simple antigen test kits and rapid PCR tests such as the LAMP method.
These tests are believed to be able to detect viral RNA levels of 50-100 copies. Although the sensitivity is somewhat lower than that of PCR tests, it is not considered a problem in practical terms in determining whether or not someone is actually infectious.
As shown below, antigen test kits and rapid PCR tests such as the LAMP method have been approved by the Ministry of Health, Labour and Welfare.
- The Ministry of Health, Labour and Welfare announced "PCR testing using saliva from asymptomatic individuals"
(Monday 2020, 7 17) https://www.mhlw.go.jp/stf/newpage_12488.html
- When comparing PCR tests using saliva with PCR tests using nasopharyngeal swabs, there was a high concordance rate for positive cases and a high concordance rate for negative cases.
- Both tests could give false negative results, but only in cases where the viral load was very low.
- This will make it possible to use saliva-based PCR tests, LAMP tests, and quantitative antigen tests on asymptomatic individuals.
In addition, the Ministry of Health, Labour and Welfare has set the standard for asymptomatic people to be released from home quarantine as "10 days have passed since the onset of symptoms and 72 hours have passed since symptoms have improved (such as the subsidence of fever) and there is no problem without a PCR test."
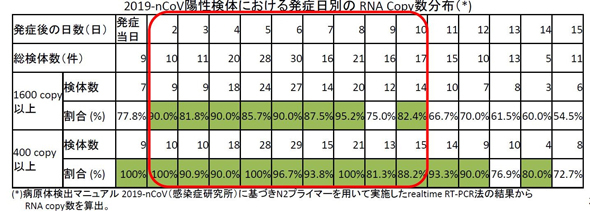
Here is some data on the amount of viral RNA, as shown below. Even on the 10th day after onset, most have over 400 copies. At this time, both PCR tests and rapid PCR tests such as antigen test kits and LAMP methods are positive.
Conversely, if the test result is "negative" within the criteria for being released from home quarantine (10 days after the onset of symptoms), it would still be reasonable to conclude that there is "no problem."
The addition of antibody testing is recommended as it will provide more information regarding past infection.
(Figure 12) From a study on the use of antigen tests based on the amount of virus by date of onset
- Simple antigen test: Fujirebio
https://www.fujirebio.co.jp/products/espline/sars-cov-2/index.html
- LAMP method (Eiken, Canon)
http://loopamp.eiken.co.jp/products/sars-cov-2/index.html
https://jp.medical.canon/products/dnachip/coronavirus
Other novel RNA tests have been reported
- SATIC method (Shionogi)
https://www.shionogi.com/content/dam/shionogi/jp/news/pdf/2020/06/200622_.pdf
*The content of this page is current as of July 2020, 9.